Overview
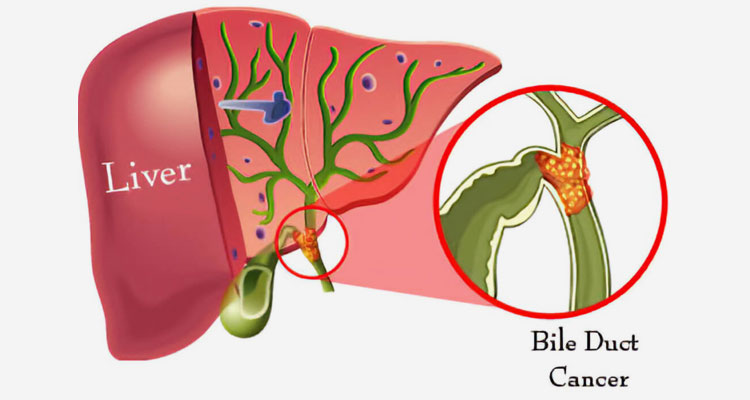
Gallbladder and bile duct
Cholangiocarcinoma is a type of cancer that forms in the slender tubes (bile ducts) that carry the digestive fluid bile. Bile ducts connect your liver to your gallbladder and to your small intestine.
Cholangiocarcinoma, also known as bile duct cancer, occurs mostly in people older than age 50, though it can occur at any age.
Doctors divide cholangiocarcinoma into different types based on where the cancer occurs in the bile ducts:
- Intrahepatic cholangiocarcinoma occurs in the parts of the bile ducts within the liver and is sometimes classified as a type of liver cancer.
- Hilar cholangiocarcinoma occurs in the bile ducts just outside of the liver. This type is also called perihilar cholangiocarcinoma.
- Distal cholangiocarcinoma occurs in the portion of the bile duct nearest the small intestine. This type is also called extrahepatic cholangiocarcinoma.
Cholangiocarcinoma is often diagnosed when it’s advanced, making successful treatment difficult to achieve.
Types
- Hilar cholangiocarcinoma
Symptoms
Signs and symptoms of cholangiocarcinoma include:
- Yellowing of your skin and the whites of your eyes (jaundice)
- Intensely itchy skin
- White-colored stools
- Fatigue
- Abdominal pain on the right side, just below the ribs
- Losing weight without trying
- Fever
- Night sweats
- Dark urine
Diagnosis
If your doctor suspects cholangiocarcinoma, he or she may have you undergo one or more of the following tests:
- Liver function tests. Blood tests to measure your liver function can give your doctor clues about what’s causing your signs and symptoms.
- Tumor marker test. Checking the level of carbohydrate antigen (CA) 19-9 in your blood may give your gastro doctor additional clues about your diagnosis. CA 19-9 is a protein that’s overproduced by bile duct cancer cells.
A high level of CA 19-9 in your blood doesn’t mean you have bile duct cancer, though. This result can also occur in other bile duct diseases, such as bile duct inflammation and obstruction.
- A test to examine your bile duct with a small camera. During endoscopic retrograde cholangiopancreatography (ERCP), a thin, flexible tube equipped with a tiny camera is passed down your throat and through your digestive tract to your small intestine. The camera is used to examine the area where your bile ducts connect to your small intestine. Your doctor may also use this procedure to inject dye into the bile ducts to help them show up better on imaging tests.
- Imaging tests. Imaging tests can help your doctor see your internal organs and look for signs of cholangiocarcinoma. Techniques used to diagnose bile duct cancer include ultrasound, computerized tomography (CT) scans and magnetic resonance imaging (MRI) combined with magnetic resonance cholangiopancreatography (MRCP). MRCP is increasingly being used as a non-invasive alternative to ERCP. It offers 3D images without the need for a dye to enhance the images.
- A procedure to remove a sample of tissue for testing. A biopsy is a procedure to remove a small sample of tissue for examination under a microscope.
If the suspicious area is located very near where the bile duct joins the small intestine, your doctor may obtain a biopsy sample during ERCP. If the suspicious area is within or near the liver, your doctor may obtain a tissue sample by inserting a long needle through your skin to the affected area (fine-needle aspiration). He or she may use an imaging test, such as an endoscopic ultrasound or CT scan, to guide the needle to the precise area.
How your doctor collects a biopsy sample may influence which treatment options are available to you later. For example, if your bile duct cancer is biopsied by fine-needle aspiration, you will become ineligible for liver transplantation. Don’t hesitate to ask about your doctor’s experience with diagnosing cholangiocarcinoma.
Treatment
Treatments for cholangiocarcinoma (bile duct cancer) may include:
- Surgery. When possible, surgeons try to remove as much of the cancer as they can. For very small bile duct cancers, this involves removing part of the bile duct and joining the cut ends. For more-advanced bile duct cancers, nearby liver tissue, pancreas tissue or lymph nodes may be removed as well.
- Biliary drainage. Biliary drainage is a procedure to restore the flow of bile. It might involve placing a thin tube into the bile duct in order to drain the bile. Other strategies include bypass surgery to reroute the bile around the cancer and stents to hold open a bile duct being collapsed by cancer. Biliary drainage helps relieve signs and symptoms of cholangiocarcinoma.
Biliary drainage done by either ERCP OR EUS guided.
We put various types of stents to drain the bile duct. (Figure 4,5,6)
- Plastic
- Metallic
- EUS guided LAMS
What is biliary stenting?
Sometimes the biliary drainage procedure may be extended with the placement of a permanent plastic or metal stent across the site of the bile duct blockage. Stents are usually inserted a few days after the initial drainage procedure and they keep the narrowed duct open without the need for a catheter.
Stenting may be preceded or followed by biliary dilatation, which involves dilating a segment of bile duct with a balloon to open up the stricture.
In recent years, endoscopic ultrasonography-guided biliary drainage (EUS-BD) in patients with failed ERCP has been reported to be an alternative method to PTBD or surgical interventions.
EUS-BD is presently classified into 3 techniques as follows:
(1) EUS-guided choledocoduodenostomy (EUS-CDS);
(2)EUS-guided hepatogastrostomy (EUS-HGS); and
(3) EUS-guided antegrade (EUS-AG) approach.
- Liver transplant. Surgery to remove your liver and replace it with one from a donor (liver transplant) may be an option in certain situations for people with hilar cholangiocarcinoma. For many, a liver transplant can be a cure for hilar cholangiocarcinoma, but there is a risk that the cancer will recur after a liver transplant.
- Chemotherapy. Chemotherapy uses drugs to kill cancer cells. Chemotherapy may be used before a liver transplant. It may also be an option for people with advanced cholangiocarcinoma to help slow the disease and relieve signs and symptoms. Chemotherapy drugs can be infused into a vein so that they travel throughout the body. Or the drugs can be administered in a way so that they are delivered directly to the cancer cells.
- Radiation therapy. Radiation therapy uses high-powered energy beams from sources such as X-rays and protons to kill cancer cells. Radiation therapy can involve a machine that directs radiation beams at your body (external beam radiation). Or it can involve placing radioactive material inside your body near the site of your cancer (brachytherapy).
- Targeted drug therapy. Targeted drug treatments focus on specific abnormalities present within cancer cells. By blocking these abnormalities, targeted drug treatments can cause cancer cells to die. Your doctor may test your cancer cells to see if targeted therapy may be effective against your cholangiocarcinoma.
- Immunotherapy. Immunotherapy uses your immune system to fight cancer. Your body’s disease-fighting immune system may not attack your cancer because the cancer cells produce proteins that help them hide from the immune system cells. Immunotherapy works by interfering with that process. For cholangiocarcinoma, immunotherapy might be an option for advanced cancer when other treatments haven’t helped.
- Heating cancer cells. Radiofrequency ablation uses electric current to heat and destroy cancer cells. Using an imaging test as a guide, such as ultrasound, the doctor inserts one or more thin needles into small incisions in your abdomen. When the needles reach the cancer, they’re heated with an electric current, destroying the cancer cells.
- Photodynamic therapy. In photodynamic therapy, a light-sensitive chemical is injected into a vein and accumulates in the fast-growing cancer cells. Laser light directed at the cancer causes a chemical reaction in the cancer cells, killing them. You’ll typically need multiple treatments. Photodynamic therapy can help relieve your signs and symptoms, and it may also slow cancer growth. You’ll need to avoid sun exposure after treatments.
Because cholangiocarcinoma is a very difficult type of cancer to treat, don’t hesitate to ask about your doctor’s experience with treating the condition.
Supportive (palliative) care
Palliative care is specialized medical care that focuses on providing relief from pain and other symptoms of a serious illness. Palliative care specialists work with you, your family and your other doctors to provide an extra layer of support that complements your ongoing care. Palliative care can be used while undergoing aggressive treatments, such as surgery.
When palliative care is used along with other appropriate treatments — even soon after your diagnosis — people with cancer may feel better and may live longer.
Palliative care is provided by teams of doctors, nurses and other specially trained professionals. These teams aim to improve the quality of life for people with cancer and their families. Palliative care is not the same as hospice care or end-of-life care.