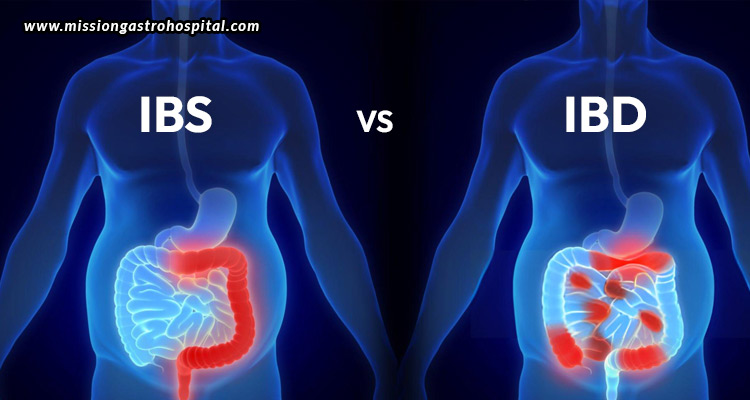
Millions of individuals worldwide suffer from two prevalent gastrointestinal conditions: inflammatory bowel disease (IBD) and irritable bowel syndrome (IBS). Even though their symptoms may be similar, they are fundamentally different conditions with unique origins, diagnostic criteria, and treatment approaches. This thorough guide will go over the main distinctions between IBS and IBD, as well as their symptoms, causes, diagnostic techniques, and management strategies.
What is IBS?
Symptoms
Functional gastrointestinal disorders, such as IBS, are typified by a number of symptoms that include discomfort or pain in the abdomen, gas and bloating, alterations in bowel habits, and mucus in the stool. These symptoms are prone to fluctuations and can be brought on by certain foods, hormone fluctuations, or stress.
Causes
Although the precise aetiology of IBS is unknown, a number of variables are believed to play a role in its development.
- Gut-brain axis dysfunction: Imbalanced gut-brain connection can affect bowel function and sensitivity.
- Intestinal motility: Constipation or diarrhoea may be brought on by abnormal muscular contractions in the intestines.
- Visceral hypersensitivity: This is the increased sensitivity of the intestines to pain or discomfort.
- Imbalance in the gut microbiota: An imbalance in the gut microbiota can cause IBS.
- Psychological factors and stress: Anxiety, sadness, and stress can intensify the symptoms of IBS.
Diagnosis
IBS can be diagnosed after ruling out other illnesses and then evaluating clinical symptoms. The Rome IV criteria, which include changes in stool frequency and shape and recurrent abdominal discomfort that has occurred at least once a week for the previous three months, are widely applied. A complete medical history, physical examination, and occasionally other tests like blood, stool, and colonoscopy are also part of the diagnosis process in order to rule out other gastrointestinal conditions including inflammatory bowel disease or celiac disease.
Management
Generally, a mix of dietary adjustments, lifestyle adjustments, and medication is used to manage IBS. For instance, reducing the intake of trigger foods, sticking to a low-FODMAP diet, and consuming more fibre can all help control symptoms. Stress reduction methods, consistent exercise, and enough sleep can all also help with symptoms. Doctors may prescribe laxatives, antidepressants, antispasmodics, and antidiarrheals, while other psychological therapies, such as cognitive-behavioural therapy (CBT), may also be helpful.
What is IBD?
Symptoms
The term “IBD” refers to a group of chronic inflammatory gastrointestinal disorders, the most common of which being ulcerative colitis and Crohn’s disease. Typical signs and symptoms include persistent diarrhoea, cramps and discomfort in the abdomen, blood in the stool, fatigue, weight loss, and reduced appetite.
Causes
Although the precise origin of IBD is unclear, a confluence of immunological, environmental, and genetic factors is thought to be responsible.
- Genetics: An increased chance of having IBD is associated with a family history of the illness.
- Immunological system dysfunction: The gastrointestinal system is attacked by an aberrant immunological response, which results in inflammation.
- Lifestyle factors: The illness may be brought on by or made worse by variables including nutrition, smoking, and infections.
Diagnosis
A combination of imaging scans, endoscopic procedures, laboratory testing, and clinical examination is used to identify the inflammatory bowel disease. Blood tests can help to look for dietary deficits, inflammation, and anaemia. Stool tests can rule out infections and identify inflammation. Imaging studies like X-rays, CT scans, and MRIs can all be used to determine the degree and site of inflammation. Finally, direct visualisation and biopsy of the gastrointestinal system can be made possible through endoscopy and colonoscopy.
Management
In order to treat IBD, inflammation must be under control, remission must be reached and maintained, and complications must be avoided. This is why it is critical to quit smoking, manage stress, and get frequent follow-up treatment. Some diets, including the Exclusive Enteral Nutrition or the Specific Carbohydrate Diet (SCD), can also help control symptoms. Doctors may also prescribe corticosteroids, immunomodulators, biologic treatments, and anti-inflammatory medications (aminosalicylates), while severe instances may require surgical intervention to remove damaged gastrointestinal system segments.
Key differences between IBS and IBD
Nature of the condition
- IBS: A functional condition in which there is no obvious gastrointestinal tract irritation or damage
- IBD: An inflammatory disease characterized by gastrointestinal tract damage and visible inflammation
Signs and symptoms
- IBS: Abdominal discomfort, bloating, and changes in bowel habits without blood in the stool
- IBD: Constant diarrhoea, discomfort in the abdomen, blood in the stool, exhaustion, and weight loss
Causes
- IBS: Multifactorial, including dysbiosis of the gut-brain axis, problems with motility, hypersensitivity, and imbalance in the microbiota
- IBD: Involves environmental causes, immune system malfunction, and genetic predisposition
Diagnosis
- IBS: Diagnosed based on the patient’s symptoms, and by ruling out other illnesses
- IBD: Identified by endoscopic procedures involving biopsies, imaging investigations, blood testing, and stool tests
Treatment
- IBS: Treated with food adjustments, lifestyle modifications, medications, and psychological therapies
- IBD: Treated with biologics, immunomodulators, anti-inflammatory medications, dietary changes, and occasionally surgery
Importance of consulting a gastroenterologist
Both IBS and IBD significantly impact quality of life, and receiving specialized treatment is necessary for efficient management of both disorders. It is important to see a gastroenterologist for a number of reasons.
- Correct diagnosis: Gastroenterologists are skilled in correctly identifying IBS, IBD, and other gastrointestinal disorders, assuring the right course of action.
- Customized treatment plans: Gastroenterologists are able to create customized treatment programmes based on the unique requirements and seriousness of the ailment.
- Advanced therapy: When necessary, gastroenterologists can provide advanced therapies such as biologic medicines and surgical techniques.
- Multidisciplinary approach: Gastroenterologists collaborate with psychologists, nutritionists, and other medical specialists to provide all-encompassing care.
- Monitoring and follow-up: Gastroenterologists can help manage the symptoms of chronic illnesses and avoid complications with regular monitoring and follow-up treatment practices.
One of Ahmedabad’s leading facilities for the treatment of gastrointestinal disorders, Mission Gastro Hospital, offers the finest possible care for patients. The hospital, with the best gastroenterologist in Ahmedabad, cutting-edge facilities, and a patient-centric approach, skilfully manages a variety of gastrointestinal disorders, while enhancing the general health and well-being of every patient.